Period pain is common. But when does it become concerning and could cancer drugs be the answer?
Lotte Weber was 16 years old when prescribed the birth control pill to treat her debilitating periods. She describes withering on the bathroom floor due to the intensity of the pain and missing multiple days of school. Doctors suspected she had endometriosis, however her youth delayed diagnosis.
“It’s a very invalidating experience when you’re going through that much pain,” she said. “Someone kind of says, 'oh, you’re a wimp'.”
Looking back at her experience as a teenager trying to get a diagnosis, Weber felt there was “medical gaslighting”. The gynaecologist who prescribed her the pill questioned her pain threshold. “I was told I’m a teenager, my body’s still getting used to my cycle. [We’ll] put you on the pill for a few years,” she said. “[For] some people it helps a lot, but not in my case.”
Weber is not alone in her experience. For many women, the pill remains the most common treatment option available for suspected endometriosis. For many women it is a successful way of managing their chronic pain. However, for those unresponsive to it, further treatment is limited and often invasive, usually requiring surgery.
Endometriosis is a chronic condition where cells similar to the lining of the uterus grow outside of the uterus. Unlike period pain, endometriosis can cause scar tissue and inflammation, usually in the pelvic region. It can also lead to infertility and impact the quality of a woman's life. Diagnosis is difficult as symptoms vary for each patient and surgery is the only method to receive an official diagnosis in the early stages of the disease.
Weber, now 20, received a diagnosis of Stage 3 endometriosis this year via a new deep ultrasound scan. For those at earlier stages of the disease, surgery is the only way to diagnose the problem as ultrasounds cannot detect microscopic early-stage forms of the disease. Accessing surgery is difficult for younger women, as doctors can be hesitant to perform surgery on teenagers, leading to a delayed diagnosis.
Endometriosis is most commonly found in the pelvis and bowel however UNSW research scientist Kate Gunther, who is writing her PhD on endometriosis, notes it can also be found in other areas of the body such as the arm and leg muscles, the lungs and in rare cases the brain.
'If the molecular causes between cancer and endometriosis are so similar, there’s no reason we can’t use some cancer drugs to treat endometriosis.'
“There was a case study where somebody found endometriosis at the top of their nasal cavity, and they only found it because they had a monthly nosebleed because those cells were also responsive to their menstrual cycle,” she said.
At present, there are limited treatment options available to patients, the most common being anti-inflammatory drugs, hormonal contraceptives such as the pill and IUDs, and surgery.
An estimated one in nine women and girls and those born female suffer from endometriosis, according to Endometriosis Australia. The pill is commonplace treatment, and for many women is a successful means of managing their chronic pain. However, Gunther notes that “about 30 per cent of people have that biology where it’s never going to work for them”.
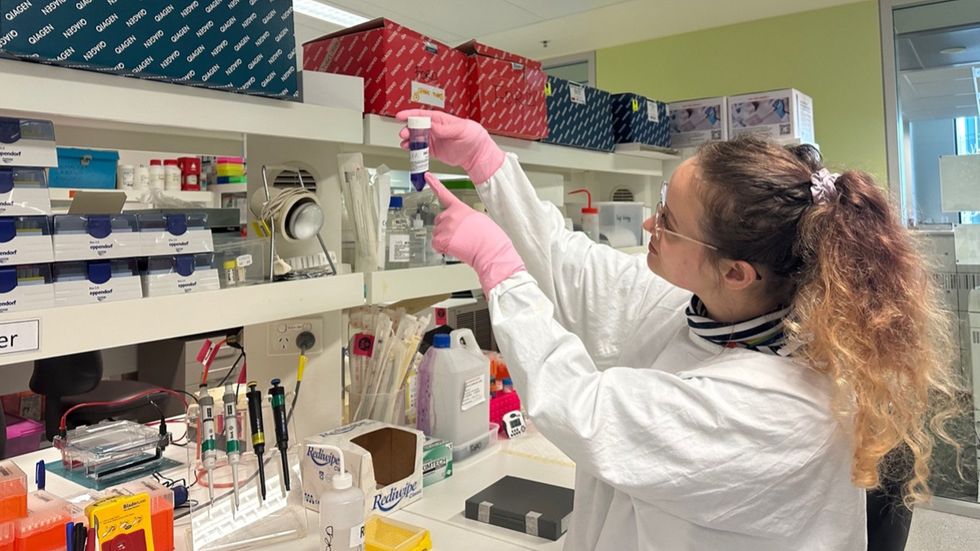
Gunther and the team at UNSW’s Gynaecological Cancer Research Group are interested in the use of “targeted agent” drugs popular in cancer treatment for endometriosis. She said endometriosis has “cancer-like properties” and shares some of the same mutated genes as cancer. Unlike chemotherapy which affects every cell in the body, Gunther said targeted agents affect only diseased cells.
“If the molecular causes between cancer and endometriosis are so similar, there’s no reason that we can’t use some cancer drugs to actually treat the endometriosis,” she said. “At the moment, there’s not too many treatment options. The treatments, quote unquote, that are available to patients frequently don’t work.”
Testing existing drugs is cost-effective and less time consuming. Research assistant Teagan Fisher at UNSW’s Gynaecological Research Group said it’s much quicker and cheaper to repurpose existing drugs that have already undergone safety testing.
“It’s actually a lot quicker than developing new drugs because all that base initial work has already been done,” she said. “All you’ve got to do is look for other targets of that drug and then see if your disease, endometriosis, also has that target. You can get it to patients a lot quicker.”
To test these drugs, Gunther and the team are working with lab models of endometriosis where tissue has been removed during surgery to replicate the disease. She said although not quite the same as treating a whole person, the diversity of tissue available allows her to see a variety of symptoms and effects of the drugs.
The team’s long-term goal is to give more personalised treatment recommendations to patients. To achieve this, Gunther said a better understanding of the biology is needed. While target-agent drugs can be used to treat cancer, more research is necessary to deem them safe for endometriosis.
“While a drug may be safe in the context of saving someone’s life from cancer, endometriosis is a chronic disease and any drugs may need to be taken for years,” she said. “We still need to better understand this before we can get to the point of prescriptions.”
Elyse Powell, a registered nurse who assists the research team at UNSW, said there are significant gaps in the science on endometriosis that are delaying drug research. “I think unfortunately the fact that it has been under-researched has failed us because we have to start from all the way back,” she said. “There’s just so much uncertainty that’s hard to tackle.”
Since July 2018, with the release of the National Action Plan for Endometriosis, the Federal Government has committed $87 million to endometriosis research, care and education. Gunther said that although more women worldwide are affected by endometriosis than diabetes and dementia combined, funding for these diseases is “four times what it is for endometriosis”.
Gunther hopes the use of targeted agent cancer drugs will allow for a specialised treatment of endometriosis with less side effects. The drugs could also offer a more equitable and accessible line of treatment for patients, as more invasive procedures like surgery can be difficult to access.
Fisher who also suffers from endometriosis said she’s had symptoms since she was 12 but only received surgery last year at age 24 to be officially diagnosed. “You’re 15 and you present these symptoms, you may not even want to consider surgery as an option,” she said. “I was about that age when my doctor first suggested it might be endometriosis, but he was like, 'I’m not going to do surgery on a teenager'.”
Weber finally had surgery this year to remove a 17cm growth. Speaking of how long it took to get the surgery, she said: “I understand that they were sort of trying to protect me from invasive procedures, but I think that a lot of medical gaslighting came into play as well.”
Despite limited treatment options and gaps in research, the future is looking brighter for endometriosis patients. Weber nods to the media attention endometriosis has garnered in recent years. “I’ve noticed lately, like Bindi Irwin… a lot of people are talking about it in quite sort of mainstream news channels at the moment, which I think is great.”
Anna is studying a double Bachelor's degree in Media (Communications and Journalism) and Law at UNSW. She is a passionate storyteller and is interested in a career in investigative journalism.





Afraid of an egg: the tyranny of living with social media's body standards